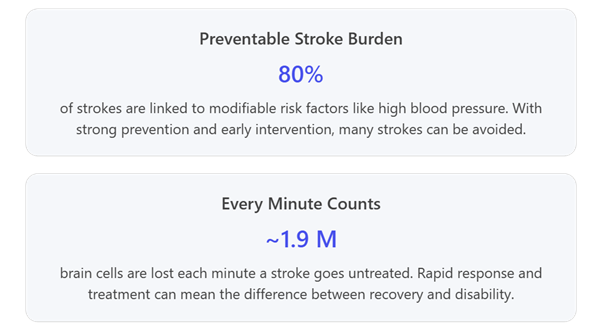
Yet today, too few patients have access to the swift, high-quality stroke care that modern medicine can provide. Time lost is brain lost. Each minute of delay between stroke onset and treatment can destroy nearly two million neurons. We have game-changing therapies – like clot-busting drugs and mechanical thrombectomy – that can stop a stroke in its tracks, dramatically improving outcomes. However, access to these innovations remains far too limited globally, especially in lower-resourced areas. This gap between what’s possible and what’s reality is what drives me as an advocate. We have the knowledge and tools to beat stroke – if we act quickly and work together to get those tools to everyone who needs them.
Progress through partnership in stroke advocacy
The good news is that in recent years, stroke has finally begun to get the policy attention it deserves, thanks to unprecedented collaboration across sectors. I’ve been fortunate to work at the crossroads of industry, medicine, and policy, and I’ve witnessed a real turning of the tide. A major catalyst was the formation of the Global Stroke Action Coalition (GSAC), which has been urging governments worldwide to make stroke a priority. Through GSAC and partnerships with groups like the World Stroke Organisation, European Stroke Organisation, SVIN, and others, we created a united front for stroke advocacy that simply didn’t exist at this scale before.
This collaboration is yielding results. Consider what’s happened on the global stage just in the past year: At the World Health Assembly 2025, health leaders from around the world gathered for a special event we helped organise – pointedly titled “Overlooked & Underfunded” – which brought together Ministers of Health from countries as diverse as Brazil, Egypt, and Bhutan and launched the “Every Minute Counts” campaign to rally urgent action on stroke. A few months later, during the United Nations General Assembly, stroke took on a prominent role in discussions on non-communicable diseases: a high-level roundtable (convened by our coalition) united ministers, NGO leaders, and industry in a call to make stroke prevention and treatment a national and international priority.
That same week, world leaders endorsed a Political Declaration on non-communicable diseases (2025) that, for the first time, explicitly recognises the need to scale up early stroke screening, treatment access, and rehabilitation in every country. Even the business community is now engaged – we took the case for investing in stroke to the World Economic Forum, co-authoring an article titled “Why It’s Time We Invested in Stroke Care” to put stroke on the radar of global business and policy leaders. The message at all these forums has been clear: if we join forces across industry, health systems, and governments, we can dramatically reduce the toll of stroke.
Crucially, policy is finally catching up with science. In 2024, the World Health Organisation released its first-ever global Framework for the care of Acute Coronary Syndrome and Stroke, which urges countries to develop national stroke plans and emphasises integrating stroke throughout the health system – from early detection and digital tools to rehabilitation.
Around the same time, the WHO officially recognised mechanical thrombectomy as a “best-buy” intervention for stroke, underscoring the need to build more stroke-capable centres with trained specialists. Here in Europe, we are on the cusp of an EU Cardiovascular Health Plan — modelled after Europe’s successful €4 billion Cancer Plan — aimed at channelling similar investment into cardiovascular disease.
The MedTech Europe Cardiovascular Sector Group, of which I am a proud member, formulated their key requests for the Health Plan. Life-saving and improving innovations enhance patient outcomes and alleviate pressure on healthcare systems. They enable earlier diagnoses, personalised interventions, and more efficient prevention and provision of care for patients suffering from all types of cardiovascular diseases (including stroke, heart failure, atrial fibrillation, structural heart disease, and vascular disease).
MedTech Europe shares the Commission’s clear and measurable objective for the Plan, namely reducing premature and preventable CVD deaths and disability in the EU by 30% by 2030, which is aligned with UN SDG 3.4. We urge the Commission to allocate €5 billion over 5 years, strategically leveraged across multiple EU instruments. To put that into perspective, this represents less than 2% of the total economic burden of €282 billion imposed annually by CVD.
A key goal of this upcoming plan is to expand the network of “stroke-ready” hospitals and thrombectomy-capable centres across EU member states, so that wherever a stroke strikes, patients can get life-saving treatment fast. And in a joint effort with the World Stroke Organisation, we recently published a WSO-Philips Global Policy Paper on Stroke (2024), which offers governments a clear roadmap: invest in dedicated stroke units and coordinated care pathways, because doing so saves lives and also saves money by reducing long-term disability costs.
There’s even talk of a dedicated World Health Assembly resolution on stroke in 2026 – something that would have been unimaginable a decade ago. All these developments signal real momentum toward the vision that motivates us: a world where every stroke patient, wherever they live, has timely access to high-quality care.
In Europe, we need to accelerate access to innovation by implementing tailored actions from early evidence that reward long-term value as part of procurement processes, accelerated regulatory pathways, and funding and reimbursement models, to ensure patients and healthcare systems can access existing and breakthrough innovations.
Technology, training and awareness: keys to better stroke outcomes
As someone working in health technology, I am encouraged by how innovations are improving stroke care. Today’s advanced imaging, AI diagnostics, and minimally invasive therapies enable doctors to make faster decisions and often halt a stroke in progress. Telehealth is bringing stroke expertise into small or remote hospitals, so that even if a stroke occurs far from a major centre, local clinicians can get instant guidance from specialists.
However, technology alone is not enough. Delivering real impact requires investing in people and systems: we need to train more stroke neurologists and interventional specialists, equip ambulance teams and emergency staff with the skills to recognise and handle strokes swiftly, and ensure every hospital has protocols aligned with the latest evidence. In our partnerships, a big focus has been on training and education – from simulation-based training programs to sharing best practices across countries – to help build local capacity for stroke care.
We must also never underestimate the power of public awareness. Often the first “responder” to a stroke is not a doctor, but a family member or bystander who recognises something’s wrong and calls emergency services. That’s why one of the simplest yet most powerful tools we promote is the acronym F.A.S.T. – Face drooping, Arm weakness, Speech difficulty, Time to call emergency. If everyone knows these telltale signs, anyone can act quickly when a stroke strikes.
Remember: most people having a stroke cannot diagnose themselves; it’s usually a loved one or colleague who witnesses the symptoms. This World Stroke Day, public campaigns around the globe are teaching millions to act F.A.S.T., and stroke survivors are sharing their stories to spread hope and knowledge. Every person educated is a potential life-saver, because in stroke care speed is everything.
A Call to Action: make stroke a priority
Despite the progress we’ve made, much work remains ahead. Now is the time to turn awareness into action. I urge policymakers everywhere to make stroke a true priority on the health agenda. This starts with recognising stroke in national health plans and committing to funded National Stroke Action Plans that cover the entire care pathway, from prevention through rehabilitation. It means investing in stroke-ready infrastructure – ensuring every region has a hospital equipped and staffed to deliver acute stroke treatments and building hub-and-spoke networks to get patients to the right facility at the right time.
We need to commit resources to proven interventions (like stroke units, thrombolysis and thrombectomy) and explore innovative financing (for example, some countries are levying health taxes on tobacco or sugar to fund stroke programs). I also call on governments to implement robust tracking – measure stroke incidence, treatment rates, and outcomes – because we can’t improve what we don’t measure. And critically, we must include stroke survivors and caregivers in policy development: their lived experience offers invaluable insights, and they deserve a seat at the table when decisions are made.
My message today is simple: the time to act on stroke is now. We have momentum, the tools, and the evidence. By prioritising stroke care – by investing in prevention, speeding up treatment, and supporting survivors – governments can save countless lives, reduce disability, and ease the enormous societal burden that stroke imposes. This is not just a healthcare issue; it’s a matter of preparing for a healthier future for our aging populations.
On this World Stroke Day, let’s commit to turning our commitments into real-world impact. I invite health leaders, policymakers, and communities everywhere to join us in this mission to transform stroke care. We’ve proven that collaboration and dedication can yield results; now we must push further. Together, we can build a world where strokes are less frequent and less devastating.
Let’s seize this moment and make it count – because when it comes to stroke, Every Minute Counts.